Human Papillomavirus – HPV – Vertical Transmission – a review of current data
Previous SectionNext Section
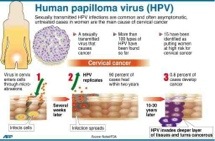
Human papillomavirus (HPV) is the most common sexually transmitted infection among humans, and represents a well-established cause of cervical cancer in females and a significant factor in the development of anogenital, head, and neck cancers [1].
A number of investigations have found that HPV infection may also be transmitted by nonsexual routes [2], as HPV DNA has been detected in blood and in reproductive and placental cells, as well as in infants, in children, and in individuals who have never had sexual intercourse [2–4]. HPV horizontal transmission through saliva or other contact has been invoked to explain cases of oral infection in infants whose mothers are HPV negative [5], and investigations of vertical transmission have led to conflicting results and transient HPV detections in children [6, 7]. Thereby, we are still unable to fully understand the clinical relevance of these findings, for either pregnancy or pediatric care.
In theory, vertical transmission can occur through the following mechanisms of transmission: periconceptual transmission (during fertilization of an oocyte or immediately after fertilization), prenatal (during pregnancy), and perinatal (during or immediately after birth). In this review, we will discuss the significance and implications of the presence of papillomavirus in nonepithelial sites, and examine the possible consequences of fetal exposure to HPV and the extent to which these new findings can provide a better understanding of the natural history of papillomavirus infection.
Previous SectionNext Section
POSSIBLE MECHANISMS OF HPV VERTICAL TRANSMISSION
Although HPV DNA has been detected in different sites of the male reproductive tract [8–10], sperm cells [4, 11, 12], semen [13, 14], endometrium, and ovaries [15], which suggests that HPV could be transmitted during the fertilization of an oocyte or immediately afterward, the significance of these findings is still unknown. In vitro analyses have indicated the viability of HPV infection in spermatozoids and the transcription of HPV genes in fecund oocytes [8–10, 16–20], and the transcriptional activity of HPV-16 in sperm was confirmed in vivo [21]. However, further investigations are necessary to confirm this route of transmission.
For this reason, the discussion about the possible mechanisms of HPV vertical transmission will center on the prenatal and perinatal routes, which are better understood.
Previous SectionNext Section
PRENATAL TRANSMISSION
The observation of infants showing signs of HPV-induced lesions at birth, such as laryngeal and anogenital lesions, has led to the belief that intrauterine HPV transmission can occur [22, 23]. HPV DNA has been detected in amniotic fluid [3], placenta, and the umbilical cord [7]. Both chorionic and placental tissue can be infected through the hematogenous route and hence, HPV can be spread to amniotic cells that are then ingested by the fetus [2, 3]. Transplacental infection, another possible means of HPV intrauterine transmission, can occur through the ascending route from the maternal genital tract, as it has been shown that the presence of HPV-DNA, both in amniotic fluid [3] and the umbilical cord [2], is correlated with cervical intraepithelial lesions in pregnant women.
Once believed to be low, the HPV vertical transmission rate has shown inconsistent results, probably due to the heterogeneous nature of the clinical trials [24]. Despite this, in a systematic quantitative review, Medeiros et al [24] reported a pooled relative risk of mother-to-child HPV transmission (4.8) when the mother is shown to be HPV positive. Additionally, the risk of the newborn having the same HPV type as that found in the maternal genital tract is 4 times greater when the umbilical cord blood is positive for the same HPV [25]. Evidence from the cervical samples indicates that mothers who transmit HPV to their infants have a higher viral load than those who do not [26].
Sarkola et al [25] reported that peripheral blood samples from all mothers who had HPV in the placenta and umbilical cord tested negative for HPV. According to these authors, the detection of viral DNA in their samples appears to be due to a maternal history of productive infection and not the detection of viral genetic material during pregnancy. However, there remains the possibility that HPV infected the placenta during early pregnancy and had already cleared the cervix at the time of delivery [2].
During pregnancy, the uterine canal undergoes anatomic and immunologic changes that may increase the susceptibility of pregnant women to infections [27]. In addition to other human viruses such as HIV, cytomegalovirus, and Epstein-Barr virus, HPV may be able to infect the placenta or cells of fetal origin [28]. The transplacental transmission of HIV and maternal cells, including lymphocytes, is a phenomenon that has already been described and can be stimulated by pathologic conditions [28, 29]. Reports of the presence of HPV in polymorphonuclear cells suggest that the transfer of maternal cells could allow the virus to pass through maternal–fetal barrier. Additionally, as observed for hepatitis B virus and herpesvirus, under certain immunosuppressive conditions, there can be an increase in the passage of lymphocytes carrying latent HPV through the maternal–fetal barrier [28].
HPV trophoblast infection has been described in different studies [25, 30, 31]. Furthermore, You et al [32] demonstrated in vitro that trophoblast cells are broadly permissive for HPV and that this virus is able to complete its life cycle in trophoblast cell cultures.
Previous SectionNext Section
PERINATAL TRANSMISSION
In this section, perinatal transmission will be considered as the result of the fetus coming into contact with infected cells of the vagina and cervix during birth. Some authors have demonstrated that there is both an increased rate of HPV detection among newborns by vaginal delivery (51.4%), compared to those delivered by cesarean section (27.3%) [33] and an increased incidence of juvenile respiratory papillomatosis after prolonged delivery (>10 hours) [34]. At the same time, Tenti et al [35] observed a low potential for viral transmission to the oropharyngeal mucosa of newborns from mothers without changes in oncotic colpocytology or a history of genital warts.
The view that a cesarean delivery provides protection against the transmission of neonatal herpes in pregnant women with obvious injuries has led to the suggestion that this procedure can be adopted for perinatal pregnant women with genital warts [27]. However, there is no clear consensus about the degree of protection that cesarean delivery can offer against maternal–fetal transmission of HPV [2]. This lack of agreement is based on 3 hypotheses: (1) the risk of disease transmission would be low; (2) a cesarean delivery does not ensure complete protection, because papillomatosis transmission has even been observed in elective cesarean delivery; and (3) the risks resulting from a cesarean section are greater than the potential benefits [5, 34]. In rare circumstances, the cesarean is recommended for women with genital warts that cause obstruction in the birth canal, or in cases where vaginal delivery will result in excessive bleeding due to laceration of the warty lesions [27].
Previous SectionNext Section
HPV VIRAL LATENCY
Given the lack of a clear understanding of the natural history of HPV, this raises a key question: Does the failure to detect viral DNA transmitted from a previously infected individual represent viral clearance or a state of viral latency [36]? In natural history studies, women may undergo multiple transient states that can lead to detection of HPV DNA in cervical samples [37]. Thus, because it is impossible to detect viral DNA in an individual, we cannot differentiate between the following states: DNA-negative individuals who are not infected and immune; DNA-negative individuals not infected and susceptible; and DNA-negative and infected individuals [36].
Viral latency has been invoked to justify this situation. This viral status, which is characterized by a significant decrease in viral protein expression and the establishment of papillomavirus DNA in the episomal form, restricts the infection to basal cells of the epithelium [38], where they remain controlled by a responsive immunologic memory [39]. However, factors that suppress the immune system allow an occurrence of viral reactivation [38], as described in studies that have detected fulminant warts in immunosuppressed individuals [39].
Animal models of papillomavirus infection have provided valuable experimental evidence for viral latency [38]. The observations obtained from cottontail rabbit papillomavirus and canine oral papillomavirus models have shown that latent viral particles are virologically active under certain conditions. This is analogous to the detection of HPV DNA in normal laryngeal epithelium of patients with recurrent respiratory papillomatosis (RRP) in remission [40]. A model of HPV latency has been proposed to carry this out [36].
The limited understanding of this scenario has clear implications for a literal interpretation of the status of HPV infection, particularly for infants. Some studies suggest that detection of HPV DNA in newborns is only persistent in the early days [35] or months [6, 26]; other authors have reported cases in which HPV persists until the first [41] and third years of life [5]. The assumption that detection of HPV in newborns, from a vertical transmission, is clinically insignificant because it may not be persistent ignores the viral latency and the real implications of this mode of transmission (Figure 1).
EVIDENCE OF PAPILLOMAVIRUS VERTICAL TRANSMISSION THROUGH ANIMAL MODELS OF INFECTION BASED ON BOVINE PAPILLOMAVIRUS
To date, no studies have clearly demonstrated HPV vertical transmission in humans. However, studies with BPV (bovine papillomavirus) have shown the most consistent data to support the viability of hematogenous and vertical transmission [42, 43].
BPV is responsible for the development of skin lesions and cancers in bovids [42, 44, 45]. BPV vertical transmission was initially suggested after viral detection in the blood of cows and their offspring [45]. These reports were followed by detection of BPV DNA in the reproductive tracts of bovids, fluids and gametes, and embryonic annexes [44–49]. After the detection of BPV protein in lymphocytes [42], this cell was postulated as a vehicle for carrying BPV to the reproductive tract [49].
Recent discoveries made by Roperto et al [43] may represent a watershed in the investigation of papillomavirus vertical transmission, as their study showed productive infection of BPV-2 in cells of the uterine epithelium and chorionic placenta. Additionally, E5 oncoprotein was characterized to form a complex with the platelet-derived growth factor β receptor (PDGFßR), both in the trophoblast cells and in bovine fetal organs [43]. This complex might be associated with an abnormal organogenesis in the embryo and an impairment of pregnancy [43]. Together, these significant findings corroborate the hypothesis of the vertical transmission of this virus.
Previous SectionNext Section
IMPLICATIONS OF HPV VERTICAL TRANSMISSION
Since the 1990s, various groups have investigated HPV vertical transmission and detected viral DNA and antibodies in both pregnant mothers and in newborns [2]. However, different techniques and methodologies for sample collection (buccal swab, cervical brush, blood) or detection of viral DNA (hybridization by Southern blotting, polymerase chain reaction) have variable sensitivities and have yielded conflicting results [2, 36]. Owing to the incomprehension of the molecular mechanisms governing viral latency and the development of natural immunity against HPV, and the failure to assess viral activity, the presence of HPV-DNA in blood and reproductive and embryonic cells was treated as a transitional marker, which represented less frequent and/or nonpersistent events.
Animal models suggest that papillomavirus can be spread to different tissues by lymphocyte infection, in particular to the reproductive tract and gametes [49]. Additionally, recent experiments with cattle confirm in vivo the viability of productive papillomavirus infection in cells of the placenta. Even though HPV-DNA was also found in lymphocytes, the outcomes of this finding need further investigation.
Nobbenhuis et al [50] showed that the first 2 trimesters of pregnancy are characterized by an increasing susceptibility to HPV. It can represent a latent HPV activated during early pregnancy. In vivo and in vitro assays have shown that the levels of steroid hormones, which characteristically rise during pregnancy, may act as HPV cofactors in epithelial proliferation [27]. This means that this “window of accessibility” may increase the exposure of the fetus to vertical transmission.
The possible implications of HPV vertical transmission are wide-ranging, given the oncogenic characteristics of HPV [1]. One of the well-characterized clinical complications is RRP, which is the development of lesions in the larynx, vocal cords, and oral and nasal mucous membranes, and in rare cases, reaches the trachea and bronchi [2, 51]. RRP has a bimodal age distribution that includes the juvenile form and an adult form [51]. Although some studies have established a relationship between juvenile RRP and the presence of maternal genital warts in 30%–50% of patients [2], the majority of children who develop this disease are born from women with no history of genital warts during pregnancy [34].
Although the results are less clear than those of RRP, the presence of HPV in semen has been linked to male infertility; asthenozoospermia has been linked to viral detection, and infertile men have a prevalent HPV infection in the spermatozoid [4, 19, 20]. The exact prevalence of HPV-DNA in sperm remains a controversial issue. HPV semen infection was found in 10% of the samples from asymptomatic men who had unprotected intercourse [13]; this figure rose to 53.8% among patients affected by genital warts and 40.9% of patients who had an HPV-positive female partner [14]. Despite our lack of a clear understanding of the role of HPV in the semen, the literature raises the possibility that spermatozoids might act as a vector in the transmission of HPV DNA. This may occur both in the cumulus cells, where it can lead to implantation failure [52], and in the embryo, where it may explain why some HPV-negative pregnant women give birth to HPV-positive infants [2]. Perino et al [53] reported an increased risk of abortion when HPV-DNA testing was positive in the female partner (40% infected vs 13.7% noninfected), which was even higher when the sperm samples of the male partner were infected (66.7% infected vs 15% not infected).
In pregnant women, the risk of HPV transplacental dissemination and the subsequent development of disorders such as hydatidiform mole and choriocarcinoma have been supported by in vitro assays. HPV has been shown to deregulate trophoblast–endometrial cell adhesion and invasion [30, 54] and this finding supports the emergence of disorders and impairments in pregnancy resulting from the action of HPV in the placenta, such as genetic abnormalities of the fetus, spontaneous abortions, and premature births [30, 31]. According to Hermonat et al [31], 60% (15/25) of the samples obtained from spontaneous abortion products and 20% (3/15) of those obtained from elective abortion products were positive for the presence of HPV E6 and E7 genes. Furthermore, HPV-16 DNA in syncytiotrophoblastic cells was detected in 29% of the samples collected from the spontaneous abortion group. Finally, the exposure of a 2-cell mouse embryo to HPV-DNA demonstrated a decrease in blastocyst formation and a reduced hatching process [55].
Interestingly, Roperto et al [43] found that E5/PDGFβR complex, which is important for the development of urinary bladder carcinogenesis, was also characterized in bovine fetal organs. Although HPV E5 protein is not characterized by the main viral oncoprotein, its action on the epidermal growth factor receptor (EGFR) and its correlation with cell cycle disorders in the epithelium [56] have already been described. If the findings obtained with BPV are extrapolated for infection in humans, it can be postulated that E5/EGFR complex is related to disorders of the embryonic attachments described in the literature. In addition to a possible relationship with pregnancy loss, HPV infection was also linked to spontaneous premature births. The HPV-DNA was detected more frequently in the extravillous trophoblast region of placentas from spontaneous preterm delivery cases (15/30) than from controls (6/30) [30]. These findings support the hypothesis that HPV infection could cause abnormal placental functions which, in turn, may partly be the origin of prematurity.
Finally, the exposure of the fetal immune system to viral antigens might reduce the postpartum immune response to viral proteins, a phenomenon that might be applicable to children who develop Burkitt lymphoma and may have antibodies against Epstein-Barr virus in the first 6 months of life [22]. Considering what has been proposed for the HPV latency model, it can also be assumed that contact between the embryo or fetus with viral antigens does not have an immediate effect such as abortion or malformation. Rather, the virus remains in a latency period until some cellular disturbance stimulates the viral activation and replication. Taken together, these hypotheses could partly explain cases in which HPV-positive women give birth to HPV-negative infants, as well as the familial tendency to develop HPV-related cancers [3].
Previous SectionNext Section
PERSPECTIVES AND CONCLUSIONS
This review discusses the current concepts with regard to HPV vertical transmission. However, it should be stressed that there is still no way to describe in detail how this phenomenon occurs. This subset of work suggests a complex network of events leading to mother-to-child HPV transmission, which could be a combination of factors linked to HPV infection during pregnancy and to the pregnant mother herself (eg, age, mode of delivery). In addition, the impact of HPV transmission on embryonic outcomes seems to depend on the precise moment of infection.
In light of this, others significant questions arise: How should we proceed when HPV DNA is identified in the mother during the pregnancy? Even on the basis of conservative clinical reasoning from which the puerperal period can reverse a greater predisposition to HPV by pregnant women, this situation seems to increase the exposure of the fetus to vertical transmission. Moreover, questions about HPV in men are also important. Should research about HPV infections be extended to the fathers during the prenatal exams? Should semen banks be subject to a screening for HPV?
The number of reports of nonepithelial tropism of HPV is still increasing, and the impact of this scenario must be investigated. Further work should focus clearly on the question of characterizing these nonsexual routes of transmission and should employ methodologies that are sensitive enough to distinguish between HPV latency and productive/active infection [2, 6]. With vaccination programs against HPV still being set up in various countries, it is crucial to have a proper understanding of the natural history of HPV.
Previous SectionNext Section
Notes
Acknowledgments. We thank Raíza Bruscky for her valuable assistance in providing the illustration for the manuscript.
Financial support. The work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, and Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco.
↵ Gomes LM, Ma Y, Ho C, McGrath CM, Nelson DB, Parry S. Placental infection with human papillomavirus is associated with spontaneous preterm delivery. Hum Reprod 2008;3:709-15.
Search Google Scholar
↵ Hermonat PL, Han L, Wendel PJ, et al. Human papillomavirus is more prevalent in first trimester spontaneously aborted products of conception compared to elective specimens. Virus Genes 1997;14:13-17.
CrossRefMedlineWeb of Science
↵ You H, Liu Y, Agrawal N, et al. Infection, replication, and cytopathology of human papillomavirus type 31 in trophoblasts. Virology 2003;316:281-9.
CrossRefMedlineWeb of Science
↵ Tseng CJ, Liang CC, Soong YK, Pao CC. Perinatal transmission of human papillomavirus in infants: relationship between infection rate and mode of delivery. Obstet Gynecol 1998;91:119-24.
CrossRefMedlineWeb of Science
↵ Silverberg MJ, Thorsen P, Lindeberg H, Grant LA, Shah KV. Condyloma in pregnancy is strongly predictive of juvenile-onset recurrent respiratory papillomatosis. Obstet Gynecol 2003;101:645-52.
CrossRefMedlineWeb of Science
↵ Tenti P, Zappatore R, Migliora P, Spinillo A, Belloni C, Carnevali L. Perinatal transmission of human papillomavirus from gravidas with latent infections. Obstet Gynecol 1999;93:475-9.
CrossRefMedlineWeb of Science
↵ Gravitt PE. The known unknowns of HPV natural history. J Clin Invest 2011;121:4593-9.
CrossRefMedlineWeb of Science
↵ Trottier H, Ferreira S, Thomann P, et al. Human papillomavirus infection and reinfection in adult women: the role of sexual activity and natural immunity. Cancer Res 2010;70:8569.
Abstract/FREE Full Text
↵ Maglennon GA, McIntosh P, Doobar J. Persistence of viral DNA in the epithelial basal layer suggests a model for papillomavirus latency following immune regression. Virology 2011;414:153-63.
CrossRefMedlineWeb of Science
↵ Schmook T, Nindl I, Ulrich C, Meyer T, Sterry W, Stockfleth E. Viral warts in organ transplant recipients: new aspects in therapy. Brit J Dermatol 2003;149:20-4.
CrossRefMedline
↵ Abramson AL, Nouri M, Mullooly V, Fisch G, Steinberg BM. Latent human papillomavirus infection is comparable in the larynx and trachea. J Med Virol 2004;72:473-7.
CrossRefMedlineWeb of Science
↵ Watts H, Koutskyb LA, Holmes KK, et al. Low risk of perinatal transmission of human papillomavirus: results from a prospective cohort study. Am J Obstet Gynecol 1998;178:365-73.
CrossRefMedlineWeb of Science
↵ Roperto S, Comazzi S, Ciusani E, et al. Peripheral blood mononuclear cells are additional sites of productive infection of bovine papillomavirus type 2. J Gen Virol 2011;92:1787-94.
Abstract/FREE Full Text
↵ Roperto S, Borzacchiello G, Esposito I, et al. Productive infection of bovine papillomavirus type 2 in the placenta of pregnant cows affected with urinary bladder tumors. PLoS One 2012;7:33569.
CrossRef
↵ Carvalho C, Freitas AC, Brunner O, et al. Bovine papillomavirus type 2 in reproductive tract and gametes of slaughtered bovine female. Braz J Microbiol 2003;34:72-3.
Search Google Scholar
↵ Freitas AC, Carvalho C, Brunner O, et al. Viral DNA sequences in peripheral blood and vertical transmission of the virus: a discussion about BPV-1. Braz J Microbiol 2003;34:76-8.
CrossRef
Yaguiu A, Carvalho C, Freitas AC, Góes LGB, Stocco dos Santos RC. Papillomatosis in cattle: in situ detection of bovine papillomavirus DNA sequences in reproductives tissues. Braz J Morphol Sci 2006;23:525-9.
Search Google Scholar
Lindsey CJ, Almeida ME, Vicari CF, et al. Bovine papillomavirus DNA in milk, blood, urine, semen and spermatozoa of bovine papillomavirus-infected animals. Genet Mol Res 2009;8:310-8.
CrossRefMedline
Silva MAR, Pontes NE, da Silva KMG, Guerra MMP, Freitas AC. Detection of bovine papillomavirus type 2 DNA in commercial frozen semen of bulls (Bos taurus). Anim Reprod Sci 2011;129:146-51.
CrossRefMedline
↵ Freitas AC, Silva MAR, Carvalho CCR, et al. Papillomavirus DNA detection in non epithelial tissues: a discussion about bovine papillomavirus. In: Mendez-Villas A., editor. Communicating current research and educational topics and trends in applied microbiology. Badajos, Spain: Formatex; 2007. p. 697-704.
Search Google Scholar
↵ Nobbenhuis MA, Helmerhorst TJ, Brule AJ, et al. High-risk human papillomavirus clearance in pregnant women: trends for lower clearance during pregnancy with a catch-up postpartum. Brit J Cancer 2002;87:75-80.
CrossRefMedlineWeb of Science
↵ Derkay CS, Wiatrak B. Recurrent respiratory papillomatosis: a review. Laryngoscope 2008;118:1236-47.
CrossRefMedlineWeb of Science
↵ Kadze R, Chan PJ, Jacobson JD, Corselli JU, King A. Temperature variable and the efficiency of sperm mediated transfection of HPV 16 DNA into cells. Asian J Androl 2002;4:169-73.
MedlineWeb of Science
↵ Perino A, Giovannelli L, Schillaci R, et al. Human papillomavirus infection in couples undergoing in vitro fertilization procedures: impact on reproductive outcomes. Fertil Steril 2011;95:1845-8.
CrossRefMedline
↵ Boulenoua S, Weyn C, Van Noppen M, Moussan AM, Favre M, Delvenne PO. Effects of HPV-16 E5, E6 and E7 proteins on survival, adhesion, migration and invasion of trophoblastic cells. Carcinogenesis 2010;31:473-80.
Abstract/FREE Full Text
↵ Henneberg AA, Patton WC, Jacobson JD, Chan PJ. Human papilloma virus DNA exposure and embryo survival is stage-specific. J Assist Reprod Genet 2006;23:255-9.
CrossRefMedline
↵ Genther-Williams SM, Disbrow GL, Schlegel R, Lee D, Threadgill DW, Lambert PF. Requirement of epidermal growth factor receptor for hyperplasia induced by E5, a high-risk human papillomavirus oncogene. Cancer Res 2005;65:6534-42.
References
↵ WHO/ICO Information Centre on HPV and Cervical Cancer (HPV Information Centre). Human papillomavirus and related cancers in the world:. summary report http://www.who.int/hpvcentre Accessed 26 September 2011.
↵ Syrjanen S. Current concepts on human papillomavirus infections in children. APMIS 2010;118:494-509.
CrossRefMedlineWeb of Science
↵ Armbruster-Moraes E, Ioshimoto LM, Leão E, Zugaib M. Presence of human papillomavirus DNA in amniotic fluids of pregnant women with cervical lesions. Gynecol Oncol 1994;54:152-8.
CrossRefMedlineWeb of Science
↵ Garolla A, Pizzol D, Foresta C. The hole of human papillomavirus on sperm function. Curr Opin Obstet Gyn 2011;23:232-7.
CrossRef
↵ Puranen MH, Yliskoski MH, Saarikoski SV, Syrjänen KJ, Syrjänen SM. Exposure of an infant to cervical human papillomavirus infection of the mother is common. Am J Obstet Gynecol 1997;176:1039-45.
CrossRefMedlineWeb of Science
↵ Castellsagué X, Drudis T, Cañadas MP, et al. Human papillomavirus (HPV) infection in pregnant women and mother-to-child transmission of genital HPV genotypes: a prospective study in Spain. BMC Infect Dis 2009;9:74.
CrossRefMedline
↵ Rombaldi RL, Serafini EP, Mandelli J, Zimmermann E, Losquiavo KP. Perinatal transmission of human papilomavirus DNA. Virol J 2009;6:83.
CrossRefMedline
↵ Griffthis TRL, Mellon JK. Human papillomavirus and urological tumours: II. Role in bladder, prostate, renal and testicular cancer. BJU Int 2000;85:211-7.
CrossRefMedlineWeb of Science
Rintala MAM, Pollanen PP, Nikkanen VP, Grénman SE, Syrjanen SM. Human papillomavirus DNA is found in the vas deferens. J Infect Dis 2002;183:1664-7.
Search Google Scholar
↵ Giovannelli L, Migliore MC, Capra G, et al. Penile, uretral and seminal sampling for diagnosis of human papillomavirus infection in men. J Clin Microbol 2007;45:248-51.
Abstract/FREE Full Text
↵ Didelot-Rousseau MN, Diafouka F, Yayo E, Kouadio LP, Monnet D, Segondy M. HPV seminal shedding among men seeking fertility evaluation in Abidjan, Ivory Coast. J Clin Virol 2007;39:153-5.
CrossRefMedline
↵ Bezold G, Politch JÁ, Kiviat NB, Kuypers JM, Wolff H, Anderson DJ. Prevalence of sexually transmissible pathogens in semen from asymptomatic male infertility patients with and without leukocytospermia. Fertil Steril 2007;87:1087-97.
CrossRefMedlineWeb of Science
↵ Foresta C, Garolla A, Zuccarello D, et al. Human papillomavirus found in sperm head of young adult males affects the progressive motility. Fertil Steril 2010;93:802-6.
CrossRefMedlineWeb of Science
↵ Foresta C, Pizzol D, Moretti A, Barzon L, Palù G, Garolla A. Clinical and prognostic significance of human papillomavirus DNA in the sperm or exfoliated cells of infertile patients and subjects with risk factors. Fertil Steril 2010;94:1723-7.
CrossRefMedline
↵ Lai CH, Hsueh S, Lin CY, et al. Human papillomavirus in benign and malignant ovarian and endometrial tissues. Int J Gynecol Pathol 1992;11:210-5.
CrossRefMedline
↵ Bodaghi S, Wood LV, Roby G, Ryder C. Could human papillomavirus be spread through blood? J Clin Microbiol 2005;43:5428-34.
Abstract/FREE Full Text
Wolff H. The biologic significance of white blood cells in semen. Fertil Steril 1995;63:1143-57.
MedlineWeb of Science
Bielanski A. Disinfection procedures for controlling microorganisms in the semen and embryos of humans and farm animals. Theriogenology 2007;68:1-22.
CrossRefMedlineWeb of Science
↵ Foresta C, Ferlin A, Bertoldo A, Patassini C, Zuccarello D, Garolla A. Human papilloma virus in the sperm cryobank: an emerging problem? Int J Androl 2010;34:242-6.
Search Google Scholar
↵ Foresta C, Patassini C, Bertoldo A, et al. Mechanism of human papillomavirus binding to human spermatozoa and fertilizing ability of infected spermatozoa. PLoS One 2011;6:e15036.
CrossRefMedline
↵ Lai YM, Yang FP, Pao CC. Human papillomavirus deoxyribonucleic acid and ribonucleic acid in seminal plasma and sperm cells. Fertil Steril 1996;65:1026-30.
MedlineWeb of Science
↵ Hajek E. Contribution to the etiology of laryngeal papilloma in children. J Laryngol Otol 1956;70:166.
Medline
↵ Marcoux D, Nadeau K, McCuaig C, Powell J, Oligny LL. Pediatric anogenital warts: a 7-year review of children referred to a tertiary-care hospital in Montreal, Canada. Pediatr Dermatol 2006;23:199-207.
CrossRefMedlineWeb of Science
↵ Medeiros LR, Ethur ABM, Hilgert JB, et al. Vertical transmission of the human papillomavirus: a systematic quantitative review. Cad Saude Publica 2005;21:1006-15.
Medline
↵ Sarkola ME, Grénmani SE, Rintala MAM, Syrjanen KJ, Syrjanen SM. Human papillomavirus in the placenta and umbilical cord blood. Acta Obstet Gyn Scan 2008;87:1181-8.
CrossRef
↵ Kaye JN, Cason J, Pakarian FB, et al. Viral load as a determinant for transmission of human papillomavirus type 16 from mother to child. J Med Virol 1994;44:415-21.
MedlineWeb of Science
↵ Maluf M, Perin PM. HPV e gestação. In: Rosenblatt C, editor. HPV na pratica clinica. Atheneu: Brazil Press; 2005. p. 193-225.
Search Google Scholar
↵ Younes AS, Csire M, Kapusinszky B, Szomor K, Takács M, Berencsi G. Heterogeneous pathways of maternal-fetal transmission of human viruses. Pathol Oncol Res 2009;15:461-5.
Search Google Scholar
↵ Bhoopat L, Khunamornpong S, Sirivatanapa P, et al. Chorioamnionitis is associated with placental transmission of human immunodeficiency virus-1 genotype E in the early gestational period. Mod Pathol 2005;18:1357-64.
↵ Gomes LM, Ma Y, Ho C, McGrath CM, Nelson DB, Parry S. Placental infection with human papillomavirus is associated with spontaneous preterm delivery. Hum Reprod 2008;3:709-15.
Search Google Scholar
↵ Hermonat PL, Han L, Wendel PJ, et al. Human papillomavirus is more prevalent in first trimester spontaneously aborted products of conception compared to elective specimens. Virus Genes 1997;14:13-17.
CrossRefMedlineWeb of Science
↵ You H, Liu Y, Agrawal N, et al. Infection, replication, and cytopathology of human papillomavirus type 31 in trophoblasts. Virology 2003;316:281-9.
CrossRefMedlineWeb of Science
↵ Tseng CJ, Liang CC, Soong YK, Pao CC. Perinatal transmission of human papillomavirus in infants: relationship between infection rate and mode of delivery. Obstet Gynecol 1998;91:119-24.
CrossRefMedlineWeb of Science
↵ Silverberg MJ, Thorsen P, Lindeberg H, Grant LA, Shah KV. Condyloma in pregnancy is strongly predictive of juvenile-onset recurrent respiratory papillomatosis. Obstet Gynecol 2003;101:645-52.
CrossRefMedlineWeb of Science
↵ Tenti P, Zappatore R, Migliora P, Spinillo A, Belloni C, Carnevali L. Perinatal transmission of human papillomavirus from gravidas with latent infections. Obstet Gynecol 1999;93:475-9.
CrossRefMedlineWeb of Science
↵ Gravitt PE. The known unknowns of HPV natural history. J Clin Invest 2011;121:4593-9.
CrossRefMedlineWeb of Science
↵ Trottier H, Ferreira S, Thomann P, et al. Human papillomavirus infection and reinfection in adult women: the role of sexual activity and natural immunity. Cancer Res 2010;70:8569.
Abstract/FREE Full Text
↵ Maglennon GA, McIntosh P, Doobar J. Persistence of viral DNA in the epithelial basal layer suggests a model for papillomavirus latency following immune regression. Virology 2011;414:153-63.
CrossRefMedlineWeb of Science
↵ Schmook T, Nindl I, Ulrich C, Meyer T, Sterry W, Stockfleth E. Viral warts in organ transplant recipients: new aspects in therapy. Brit J Dermatol 2003;149:20-4.
CrossRefMedline
↵ Abramson AL, Nouri M, Mullooly V, Fisch G, Steinberg BM. Latent human papillomavirus infection is comparable in the larynx and trachea. J Med Virol 2004;72:473-7.
CrossRefMedlineWeb of Science
↵ Watts H, Koutskyb LA, Holmes KK, et al. Low risk of perinatal transmission of human papillomavirus: results from a prospective cohort study. Am J Obstet Gynecol 1998;178:365-73.
CrossRefMedlineWeb of Science
↵ Roperto S, Comazzi S, Ciusani E, et al. Peripheral blood mononuclear cells are additional sites of productive infection of bovine papillomavirus type 2. J Gen Virol 2011;92:1787-94.
Abstract/FREE Full Text
↵ Roperto S, Borzacchiello G, Esposito I, et al. Productive infection of bovine papillomavirus type 2 in the placenta of pregnant cows affected with urinary bladder tumors. PLoS One 2012;7:33569.
CrossRef
↵ Carvalho C, Freitas AC, Brunner O, et al. Bovine papillomavirus type 2 in reproductive tract and gametes of slaughtered bovine female. Braz J Microbiol 2003;34:72-3.
Search Google Scholar
↵ Freitas AC, Carvalho C, Brunner O, et al. Viral DNA sequences in peripheral blood and vertical transmission of the virus: a discussion about BPV-1. Braz J Microbiol 2003;34:76-8.
CrossRef
Yaguiu A, Carvalho C, Freitas AC, Góes LGB, Stocco dos Santos RC. Papillomatosis in cattle: in situ detection of bovine papillomavirus DNA sequences in reproductives tissues. Braz J Morphol Sci 2006;23:525-9.
Search Google Scholar
Lindsey CJ, Almeida ME, Vicari CF, et al. Bovine papillomavirus DNA in milk, blood, urine, semen and spermatozoa of bovine papillomavirus-infected animals. Genet Mol Res 2009;8:310-8.
CrossRefMedline
Silva MAR, Pontes NE, da Silva KMG, Guerra MMP, Freitas AC. Detection of bovine papillomavirus type 2 DNA in commercial frozen semen of bulls (Bos taurus). Anim Reprod Sci 2011;129:146-51.
CrossRefMedline
↵ Freitas AC, Silva MAR, Carvalho CCR, et al. Papillomavirus DNA detection in non epithelial tissues: a discussion about bovine papillomavirus. In: Mendez-Villas A., editor. Communicating current research and educational topics and trends in applied microbiology. Badajos, Spain: Formatex; 2007. p. 697-704.
Search Google Scholar
↵ Nobbenhuis MA, Helmerhorst TJ, Brule AJ, et al. High-risk human papillomavirus clearance in pregnant women: trends for lower clearance during pregnancy with a catch-up postpartum. Brit J Cancer 2002;87:75-80.
CrossRefMedlineWeb of Science
↵ Derkay CS, Wiatrak B. Recurrent respiratory papillomatosis: a review. Laryngoscope 2008;118:1236-47.
CrossRefMedlineWeb of Science
↵ Kadze R, Chan PJ, Jacobson JD, Corselli JU, King A. Temperature variable and the efficiency of sperm mediated transfection of HPV 16 DNA into cells. Asian J Androl 2002;4:169-73.
MedlineWeb of Science
↵ Perino A, Giovannelli L, Schillaci R, et al. Human papillomavirus infection in couples undergoing in vitro fertilization procedures: impact on reproductive outcomes. Fertil Steril 2011;95:1845-8.
CrossRefMedline
↵ Boulenoua S, Weyn C, Van Noppen M, Moussan AM, Favre M, Delvenne PO. Effects of HPV-16 E5, E6 and E7 proteins on survival, adhesion, migration and invasion of trophoblastic cells. Carcinogenesis 2010;31:473-80.
Abstract/FREE Full Text
↵ Henneberg AA, Patton WC, Jacobson JD, Chan PJ. Human papilloma virus DNA exposure and embryo survival is stage-specific. J Assist Reprod Genet 2006;23:255-9.
CrossRefMedline
↵ Genther-Williams SM, Disbrow GL, Schlegel R, Lee D, Threadgill DW, Lambert PF. Requirement of epidermal growth factor receptor for hyperplasia induced by E5, a high-risk human papillomavirus oncogene. Cancer Res 2005;65:6534-42.
A. C. Freitas, F. C. Mariz, M. A. R. Silva, and A. L. S. Jesus
Department of Genetics, Federal University of Pernambuco, Recife, Brazil
Correspondence: A. C. Freitas, PhD, Av. Prof. Moraes Rego 1235, Cidade Universitária, Recife 50670-901, PE, Brazil (acf_ufpe@yahoo.com.br).
Source IDSA – clinical infectious diseases