7 Ways To Preserve The Miracle Of Antibiotics
Antibiotics are a true miracle of modern medicine. However, in reference to penicillin, the drug he discovered, Fleming gave warning in 1946 [1] that
the public will demand [the drug and] … then will begin an era … of abuses. The microbes are educated to resist penicillin and a host of penicillin-fast organisms is bred out which can be passed to other individuals and perhaps from there to others until they reach someone who gets a septicemia or a pneumonia which penicillin cannot save. In such a case the thoughtless person playing with penicillin treatment is morally responsible for the death of the man who finally succumbs to infection with the penicillin-resistant organism. I hope the evil can be averted.
Unfortunately, Fleming’s warning was unheeded, so this miracle of antibiotics is now endangered owing to the rapid escalation of antibiotic resistance combined with the equally rapid decline in discovery and development of new antibiotics.
This is now considered a global health crisis [2], and the reason is not difficult to understand. Resistance within all microbial classes continues to grow by natural evolution driven by massive use of agents that apply selective antimicrobial pressure. Pharmaceutical development that previously kept us ahead of resistance is now stalled due to economic and regulatory barriers. Fifteen of 18 large pharmaceutical companies have totally left the antibiotic field, and there has been no new class of antibiotics for gram-negative bacilli in 4 decades; only 2 drugs with new microbial targets (linezolid and daptomycin) have been introduced since 1998 [3]. The pipeline is sparse, the problem is global, and the prognosis is poor.
It is our impression that the potential for antibiotic abuse and resistance in the United States is potentially catastrophic. But it also seems clear that we could do much better with a bundled program with interventions that have established merit. These are particularly attractive in the era of healthcare reform, which prioritizes saving lives and saving money, as the cost and consequences of antibiotic resistance are enormous. What follows is not an in-depth review, but rather a summary of some major, sometimes humbling, relevant observations (Table 1) [4–17], with 7 major interventions that collectively address the multitude of contributing factors.
Table 1.
Compelling Issues From Diverse Sources Indicating the Magnitude of the Antibiotic Challenge and Opportunities in the United States
Our proposed “antibiotic salvage bundle” would include the following steps:
Establish a US database for antibiotic use and resistance comparable to that of the European Union;
Restrict use of antibiotics in agriculture;
Prevent selected nosocomial infections using an established systematic implementation plan based on precedent;
Aggressively promote antibiotic stewardship;
Promote use of new diagnostics with emphasis on point-of-care molecular methods;
Reduce the Food and Drug Administration (FDA) antibiotic barrier; and
Facilitate public–private partnerships for antibiotic development.
Previous SectionNext Section
LESSONS FROM THE EUROPEAN UNION TO DEFINE AND IMPLEMENT PRIORITIES
The European Union (EU) recognized the impending crisis of antibiotic resistance and established methods for surveillance on antibiotic use and resistance more than 15 years ago. Antibiotic use is reported as daily drug dose (DDD) per 1000 inhabitants per day according to pharmacy records, and resistance data are reported by sentinel laboratories using standard methods. The result is a living record of country-specific data for antibiotic consumption and resistance profiles by microbial species, drug, and date for 26 countries [18]. The United States has no comparable data system, but the European Union record suggests we should.
The correlation between antibiotic consumption and resistance is illustrated by comparing data for methicillin-resistant Staphylococcus aureus (MRSA) and carbapenemase-producing Klebsiella for the Netherlands versus Greece, 2 countries that are at the low versus high end, respectively, of per capita antibiotic use in the EU database (Table 2) [19, 20]. The difference is expected, but the magnitude is dramatic. The obvious result is the relative safety and limited need for new antibiotics in hospitals in the Netherlands, presumably reflecting policies and practices that foster prudent antibiotic use and infection control [16, 19].
Table 2.
Antibiotic Use and Antibiotic Resistance Rates for Methicillin-Resistant Staphylococcus aureus and Carbapenemase-Producing Klebsiella Bacteremia Isolates
An example of the use of EU data is France, which had high rates of multidrug-resistant Streptococcus pneumoniae in 2002 and also had the highest rate of antibiotic use in the European Union (36.5 DDD/1000 inhabitants) [21]. This led to an ambitious nationwide program directed to both providers and consumers. The results showed a 26% nationwide decrease in antibiotic prescriptions during the study period [21], and a follow-up report of the global antibiotic market showed that France is the country with the greatest reduction in antibiotic prescriptions in the world—a decrease of 21% from 2000 to 2009 [5].
The European Union systematically assesses antibiotic usage and resistance data to guide interventions to effect systematic change [11, 18, 19] and accomplishes this despite great diversity in resources, language, and politics (http://www.ema.europa.eu). The United States has a number of surveillance systems in place that provide relevant data, but nothing that is nearly as comprehensive or effective as the EU system. The Centers for Disease Control and Prevention (CDC) has initiated a plan that addresses some of these issues, but the lack of incentives from credentialing agencies such as The Joint Commission (a nonprofit organization that accredits and certifies healthcare organizations and programs in the United States) or funding agencies such as the Centers for Medicare and Medicaid Services are likely to limit use. It seems unacceptable and embarrassing that the United States at present does not have the necessary support to implement this plan. The Strategies to Address Antimicrobial Resistance Act was introduced to Congress nearly 6 years ago to address this need but has never come to a vote. It should be passed.
An astonishing 80% of all antibiotics sold in the United States are administered to food animals, primarily for growth promotion and infection prophylaxis [4, 22]. There is good evidence that this practice has consequences to human health and has no clear benefit to farmers, although quantitation of this effect is not possible due to the enormity of the dispersal area from run-off and other sources of environmental contamination. [23]. The direct effect was noted >35 years ago, with high rates of antibiotic resistance in the intestinal flora of farm animals and farmers [18], and more recently with molecular methods that show that resistant bacteria in farm animals do reach consumers in meat products [24]. The indirect impact is supported by observations that up to 90% of antibiotics given to animals are excreted in urine and stool and then widely dispersed through fertilizer, surface runoff, and groundwater, with a profound impact on the environmental microbiome [24]. Country-specific bans on antibiotic abuse in farm animals in the European Union have been accompanied by significant declines in antibiotic resistance in humans and animals without documented harm to humans or animals [23]. The European Union has recently requested all member states to require antibiotic prescriptions for all antibiotic use in farm animals [11]. Similar restrictions are proposed by the Institute of Medicine in the United States and by the World Health Organization [2]. The FDA has recently announced a ban on cephalosporins for growth promotion in certain livestock. A more expansive ban of nearly all antibiotic use for growth promotion is included in the proposed legislation known as the Preservation of Antibiotics for Medical Treatment Act (PAMTA; hppt://www.louise.house.gov/index.php option=com content&id=1315<emid=38). Similarly, new legislation known as the Delivering Antibiotic Transparency in Animals (DATA) Act (http://waxman.house.gov/press-release/rep-waxman-introduce-legislation-monitor-antibiotic-use-animals) would require public reporting of types and amounts of antibiotics administered to feed animals, including via feed mills. Both DATA and PAMTA should be passed.
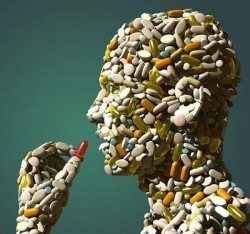
Image – enviroshow
Authors –
John G. Bartlett1, David N. Gilbert2, and Brad Spellberg3
1Johns Hopkins University School of Medicine, Baltimore, Maryland
2Department of Medical Education, Providence Portland Medical Center, Portland, Oregon
3Liu Vaccine Center, Torrance, California
Correspondence: John G. Bartlett, MD, Division of Infectious Diseases, Johns Hopkins University School of Medicine, 1830 E Monument St, Rm 447, Baltimore, MD 21205 (jb@jhmi.edu).
Source – IDSA – clinical infectious diseases